Choosing the Right Type of Orthotics: A Guide for Patients
Whether they are custom made or bought off the shelf, orthotics are a great way to alleviate pain in your feet, knees, hips, back, and even your neck and shoulders. This is because they help to distribute weight evenly so that one foot or muscle is not carrying too much of the burden.
Additionally, orthotics can improve alignment and provide support to arches, which can prevent overpronation or supination, leading to a more stable and balanced gait. However, choosing the right type of orthotics for your specific needs can be a daunting task given the variety of options available in the market. Factors such as foot shape, the severity of your condition, and the activities you engage in regularly all play crucial roles in determining the most suitable orthotic for you. To make an informed decision, it’s essential to understand the different types of orthotics and their respective benefits. Read on to gain insights into selecting the perfect orthotics to address your discomfort and enhance your overall well-being.

Customisation
Orthotics are used by doctors to help people with problems that affect the feet, ankles, and lower legs. They are often one part of a treatment plan that can also include things like more supportive shoes, physical therapy, and avoiding high impact activities.
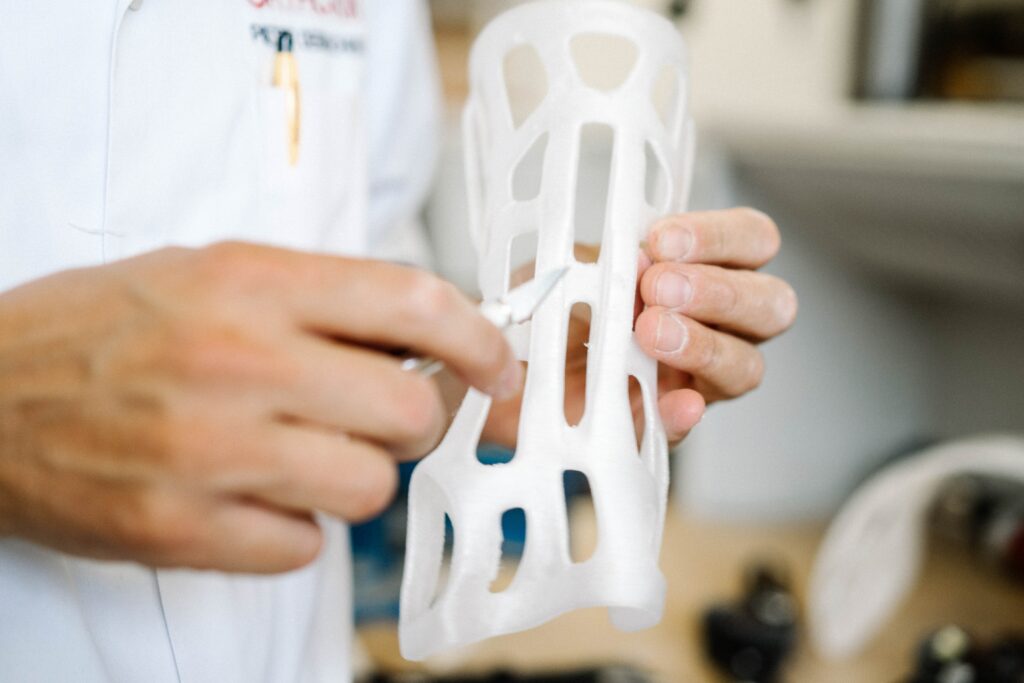
Most Melbourne orthotics are designed to support, protect, or cushion areas of the foot that are painful or uncomfortable. They can also help with alignment and improve the way the lower leg moves. They can be soft or rigid and made from a variety of materials. Some are made from a combination of materials while others are designed for specific sports such as running or skating.
The type of orthotic you need will depend on your problem. Functional orthotics are designed to move the foot in more desirable positions, while accommodative ones relieve pressure by taking stress off the feet and redistributing it to other parts of the body. Rigid orthotics are made from hard materials such as plastic or graphite while softer orthotics are usually made from flexible or semi-flexible material.
Unlike store-bought inserts, custom orthotics come with a medical evaluation and a custom fit. They can be expensive, but they come with the peace of mind that you have a device specifically designed for you. Plus, they may be covered by your insurance.
Pre-made
Most people walk into a podiatry clinic with either a strong opinion about orthotics – they don’t want to get them or they must have them. This is usually based on their own experiences, what they’ve been told, or what they read online.
Orthotics can be a great tool to use for the treatment of a variety of foot problems and injuries so that more invasive treatments like surgery aren’t needed. They can help provide cushioning to reduce painful areas and alter the force working on the foot so that it can better align or function more efficiently.
Choosing the right type of pre-made orthotics for your needs is important. While off-the-shelf orthotics are available in most stores, there are many different types and sizes and it can be difficult to find the one that fits well. They can also vary in the amount of cushioning, support, and rigidity they offer.
Over-the-counter devices are designed for the ‘average’ foot and may have features like gel or memory foam padding and constructed arch supports. However, they do not address the specific dysfunctional biomechanics of your feet and will not provide the level of correction that custom molded orthotics can provide. If you’re interested in getting pre-made orthotics, a face-to-face consultation with a qualified provider is essential to make sure the device you choose will be able to meet your needs.
Materials
Choosing the right materials is central to making the best orthotics. Different thermoplastic materials can be used to tailor the device according to a patient’s specific needs and can have a major impact on the final device’s design, comfort, and function.
A patient’s activity level and lifestyle should influence the type of material used. For example, if a patient is a runner or a weekend warrior, they may need to choose a harder or more durable type of material. This will prevent the device from collapsing in the shoe, causing discomfort and potentially damaging the foot or ankle.
Rigid materials like plastic and carbon fiber are good for addressing biomechanical problems, such as overpronation. On the other hand, soft materials such as polyethylene and EVA foam are great for diabetic and arthritic patients who need a combination of rigidity and cushioning.
The bottom cover is also important, as it will determine how well the device fits into a shoe and prevent squeaking in the shoe. Generally, this is made from a waterproof or water-resistant fabric such as neoprene, marine-grade material, or even leather.
Fit
Whether you’re a runner, a hiker, or just someone who needs to stand for long periods, foot orthotics can help. The rigid braces stabilise the ankle and foot to reduce sway and improve balance, especially for people who are overweight. They can also help relieve the pain of foot conditions like plantar fasciitis, flat feet, or fallen arches.
However, it’s important to be careful when selecting a pair of orthotics. Those purchased at a store or kiosk are often generic and may not address your specific issue. Also, the material of the orthotic can have an effect on your comfort level. For instance, soft or cushioned orthotics tend to be more comfortable while firmer ones provide better support.
You can get orthotics from a podiatrist, who can assess your foot condition and advise you on the best type for you. He or she will ask about your symptoms, when they started and what makes them worse. They will then conduct a physical exam and look at your foot alignment.
The type of orthotic prescribed will depend on your condition and other factors, such as your shoe size and lifestyle. If you’re a runner, for example, your podiatrist may recommend a specific kind of orthotic to help reduce stress on the knees during running. In other cases, the orthotics will be designed to treat a particular foot complaint, such as heel pain or overpronation.
Selecting the right type of orthotics can significantly improve your comfort and overall well-being by alleviating pain and enhancing alignment. Whether you opt for custom-made orthotics or pre-made ones, it’s crucial to consider factors such as foot shape, condition severity, and lifestyle to ensure the best fit and functionality. To receive personalised guidance and professional assessment for your orthotic needs, book an appointment with Melbourne Podiatrists and Orthotics at www.melbournepodiatristsandorthotics.com.au. Their experienced team can assist you in selecting the perfect orthotics tailored to your individual requirements, ensuring lasting relief and improved mobility.































 Podiatrists specialize in the care of feet and ankles. They treat a variety of foot and ankle conditions, including arthritis, bunions, foot deformities, sprains, and infections. They can also prescribe orthotics and braces to help patients heal. In some cases, they perform surgeries to correct certain foot and ankle problems.
Podiatrists specialize in the care of feet and ankles. They treat a variety of foot and ankle conditions, including arthritis, bunions, foot deformities, sprains, and infections. They can also prescribe orthotics and braces to help patients heal. In some cases, they perform surgeries to correct certain foot and ankle problems.




 You may be wondering if you need to have breast reduction surgery. Having large breasts can make it difficult to perform daily tasks and can negatively affect your posture. Breast reduction surgery can help alleviate these symptoms. Large breasts can also restrict your breathing. This can cause you to have trouble doing basic tasks, including sleeping.
You may be wondering if you need to have breast reduction surgery. Having large breasts can make it difficult to perform daily tasks and can negatively affect your posture. Breast reduction surgery can help alleviate these symptoms. Large breasts can also restrict your breathing. This can cause you to have trouble doing basic tasks, including sleeping.





